Abstract
Introduction: CD19 CAR-T therapy is effective for B-cell ALL. However, whether patients (pts) with EMD, High Leukemia Burden (HLB), TP53 mutation, BCR-ABL (+) mutation, or post-allogeneic hematopoietic stem cell transplantation (allo-HSCT) relapse can benefit from the treatment remains to be investigated. Here we show the efficacy and safety of CD 19 CAR-T therapy for these subgroups.
Patients and Methods: From April 2017 to April 2018 with a median follow-up of 172 (27-325) days, 83 pts with refractory or relapsed (R/R) B-cell ALL were enrolled (US NIH Clinical#:NCT03173417). The cohort included 17 with EMD, of whom 11 had central nervous system leukemia (CNSL), 13 with HLB (≥70% blast in bone marrow), 10 with BCR-ABL+, 8 with TP53 mutation, and 11 with relapsed ALL after allo-HSCT. The median age of the cohort was 10 (2-61) years. Patients' peripheral blood mononuclear cells were collected, and CD3+ T cells were separated and stimulated with CD3/CD28 dynabeads and cultured in X-VIVO 15 media with interleukin-2. T cells were transduced with a lentivirus vector encoding anti-CD19-CD3ζ either with a CD28 (21 pts) or a 4-1BB (62 pts) co-stimulatory domain, and cultured (8-10 days) until there were sufficient cells. All pts received a conditioning regimen of IV fludarabine (25 mg/m2/day) and cyclophosphamide (250 mg/m2/day) for 3 days before a single infusion of CAR-T cells with a median dose of 1x105 (0.1-10x105) cells/kg.
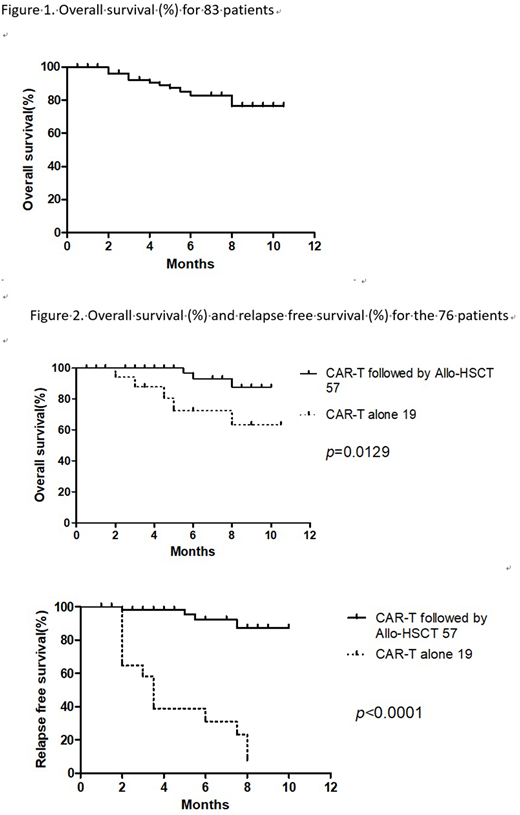
Results: On day 30 after CAR-T, 76/83 (91.6%) pts achieved complete remission (CR) or CR with incomplete count recovery (CRi), and 70/76 (92.1%) achieved minimal residual disease (MRD)-negative CR. One-year overall survival (OS) was 76.5% (Fig. 1) and relapse-free survival (RFS) was 62.6%. Grade 0-II cytokine release syndrome (CRS) incidence was 82%, and grade III-IV, 16%. There was one CAR-T-related death. Severe CNS reaction occurred in 10 pts (12%). CR was achieved in 82.4% (14/17) of pts with EMD, including 11 pts with CNSL, who had a CR rate of 82% (9/11). Incidence of severe CRS (esp. CNS toxicity) in CNSL group was not significantly increased. No significant difference in RFS was seen between pts with or without EMD (54.9% vs. 66.3%, p=0.6). However, OS (45.1% vs 88.3%, p=0.0003) favored those without EMD. 13 pts with HLB achieved 76.9% CR/CRi. Severe CRS occurred more frequently in HLB pts vs. low leukemia burden (LLB) pts (46.2% vs. 7.1%, p = 0.001). The risk was controllable.
No significant difference in CR/CRi (76.9% vs. 90.4, p=0.07) or RFS (61.1% vs 70%, p=0.55) was seen between the HLB and LLB pts, but the OS in HLB pts was inferior (54.9% vs. 80.8%, p=0.03). There was no difference in CR/OS/RFS between pts with or without the BCR-ABL mutation, including pts with 3 cases of chronic myeloid leukemia (CML) transformed into B-ALL. 88% (7/8) pts with TP53 mutation achieved CR/CRi, but only 3/7 remained leukemia free. The OS (45.7% vs. 79.5%, p=0.026) and RFS (0% vs. 67.9%, p=0.0023) were much lower for pts with TP53 mutation. 11 pts with relapsed ALL after allo-HSCT achieved 91% CR/CRi after CAR-T. The OS was similar to those treated with CAR-T before allo-HSCT (77.8% vs. 77.1%, p=0.85), with 3 pts remaining in CR by 8-12 months after CAR-T. No significant GVHD developed in these pts. Of 76 pts with D30 CR, 57 underwent subsequent allo-HSCT in a median time of 2 months post CR. The remaining 19 (including 10 post-HSCT CAR-T-treated pts) did not undergo transplant. The 1-year OS/RFS (Fig. 2) of the CAR-T bridge to allo-HSCT group was better than that of the non-transplant group (OS 87.5% vs. 63.4%, p=0.013; RFS 87.4% vs. 7.5%, p=0.001). There was a trend towards improved in OS (83.7% vs. 50%, p=0.68) and RFS (64.9% vs. 30%, p=0.18) in the MRD(-)CR group vs. the MRD(+)CR group. While the OS of CR pts was significantly better than that of CRi pts (100% vs. 73.4%, p=0.038), the RFS was not yet statistically significant (75% vs. 56.4%, p=0.25). The median recurrence time in the group without additional allo-HCST was 100 days.
Conclusion: High CR rate was achieved from CAR-T for R/R B-ALL including pts with high-risk features such as EMD, HLB, BCR-ABL+, TP53+,and relapse after allo-HSCT. CRS was manageable. CNSL is not a contraindication for CAR-T therapy. An early and high relapse rate was observed in TP53+ group. Overall, RFS was superior for pts bridging to allo-HSCT after CAR-T treatment than for those receiving CAR-T- treatment only.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal